How to Submit a Claim
Both the member’s ID Card and the verification forms contain more specific information, including the electronic payor ID needed for submitting claims. These standard claim submission instructions are also provided when providers access the Benefit Verification system:
Enter Member Information
Submit a claim for consideration through the provider portal (must include Group #, Unique ID or Insured’s Social Security number)
Enter Provider Information
Complete provider portion of the form
Enter Billing Information
Attach bills or services rendered for reimbursement
Send to Administrator
Send to Claims Administrator at the address listed on the ID Card

First-Time Users: Please call 800.634.0173 and follow the prompts to speak with a service team member to obtain a registration code and portal access.
Clearinghouse Submission Issues
We are aware of rejections due to disconnects between clearinghouses; we recommend as an interim solution providers consider utilizing Availity to submit transactions directly to us. Providers can use the attached documentation to register for Essentials to submit directly.
Availity has a 24 hour support line at 1.800.AVAILITY (1.800.242.4548) who are trained expressly in supporting providers.
ID Cards
J.P. Farley Corporation provides plan administration for a wide variety of self-funded health plans. This makes it critical for providers to reference the information provided on each member’s ID Card. Follow the instructions on the ID card to obtain member eligibility or register for online access to all relevant information through our online Provider Portal.
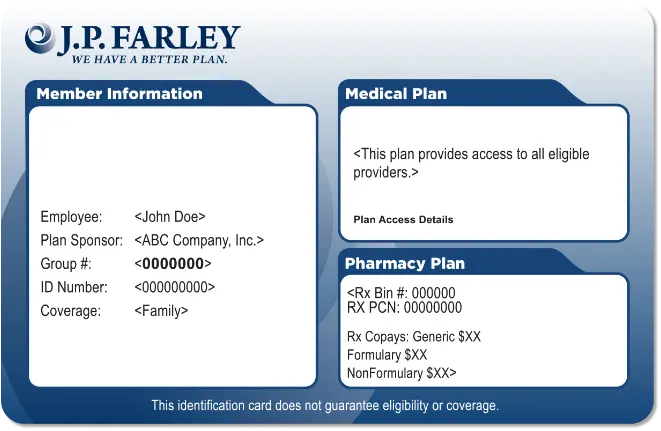
Front
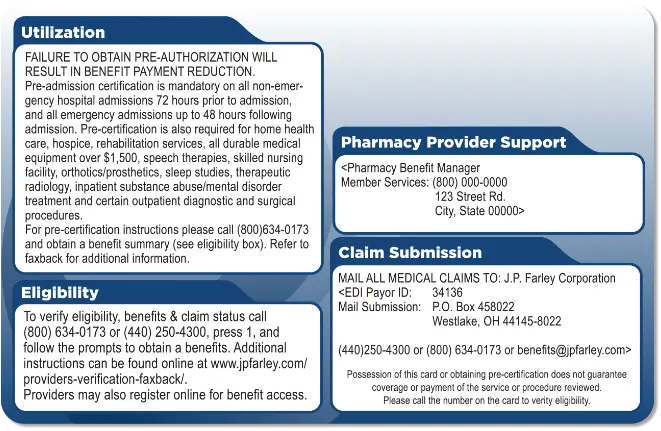
Back
When to File a Claim
Benefits are based on the Plan’s provisions at the time the charges were incurred. Claims should be filed as dictated by the terms of the plan for processing with all necessary information for proper consideration. Refer to the terms of the plan document for exact plan filing requirements.

Assignment of Benefits
By accepting assignment of benefits, the provider of services assumes both the right to payment by the Plan for services performed and accepts the limits of the Plan along with any defined deductibles and co-insurance that is required by the covered person as payment in full for the services rendered and billed for. The provider of services agrees to forgo reimbursements from the Plan or the Participant for amounts billed for the services that are in excess of what the amount the Plan allows, plus any co-insurance required by the Covered Person.
Claims payments may be audited, adjusted, negotiated and/or re-priced to minimize overpayment of claims in excess of Plan allowances. If the provider does not accept assignment of benefits as payment in full, benefit will be 100% of the Medicare allowable amount, determined based on the date of service.





